Peer Reviewed
Management of Recurrent Clostridium difficile Infection: A Case-Based Approach
Authors:
Eiyu Matsumoto, MB; Jennifer R. Carlson, PA-C; and Alice Xu, MD
Citation:
Matsumoto E, Carlson JR. Management of recurrent Clostridium difficile infection: a case-based approach. Consultant. 2017;57(10):583-587.
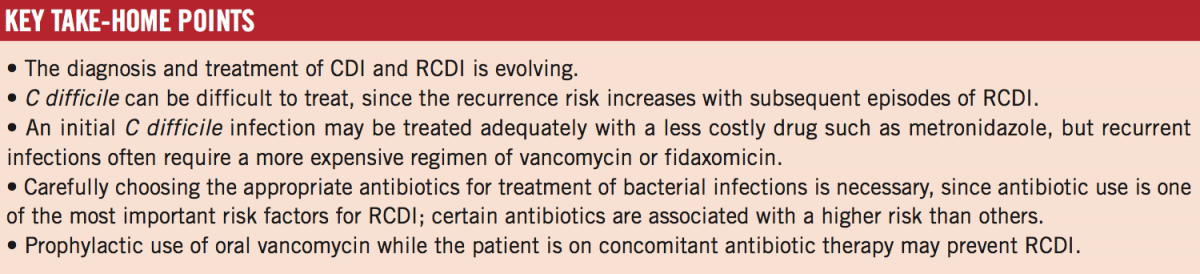
ABSTRACT: Clostridium difficile infection (CDI) is the leading cause of nosocomial diarrhea. Infection with this anaerobic spore-forming bacterium is associated with substantial morbidity and mortality. Recurrence of CDI (RCDI) is common, occurring in 10% to 20% of cases. Although 3 clinical treatment guidelines exist, the clinical outcomes for RCDI cases have been unsatisfactory. Nevertheless, advances in CDI and RCDI research have been rapid and multidirectional. This article summarizes the current standard treatment, newly reported clinical data, and anticipated research in development regarding RCDI. Two cases of RCDI are also presented.
KEYWORDS: Clostridium difficile infection, recurrent Clostridium difficile infection, antibiotics, vancomycin
Clostridium difficile is an anaerobic spore-forming bacterium. C difficile infection (CDI) is recognized as the leading cause of nosocomial diarrhea and is associated with substantial morbidity and mortality.1,2 More than 250,000 people require hospital care, and at least 14,000 people die from CDI in the United States each year.3
Recurrent CDI (RCDI) is the complete resolution of presenting symptoms on appropriate therapy followed by subsequent relapse and return of symptoms within 8 weeks of treatment completion after the initial episode.3 Approximately 10% to 20% of cases of CDI recur after the initial episode, but further recurrence rates increase to 40% to 65% after the first RCDI episode.4 Studies have shown that the majority of RCDI cases are due to relapse of infection with the original strain rather than reinfection.5,6
The main pathogenesis of RCDI is thought to be from impaired colonization resistance allowing proliferation of C difficile. Patients with RCDI have been found to have lower levels of immunoglobulins against the C difficile toxin.7 Other known risk factors for RCDI are advanced age, additional courses of antibiotics, chemotherapy, proton-pump inhibitors, prolonged hospital stay, and prior episodes of RCDI.8
The diagnosis of RCDI remains challenging. Studies have shown that enzyme immunoassay (EIA) and polymerase chain reaction assay results may remain positive for C difficile toxin A and toxin B for as long as 30 days even in patients who have symptom resolution.9,10 Therefore, testing for cure should not be performed.11-13 Fecal colonization of C difficile is common in the community and in health care facilities. Between 4% and 15% of healthy adults may be asymptomatically colonized with the pathogen.14 One study reported asymptomatic carriage rates at admission of 6% to 11% and acquisition rates of 4% to 21%, with more than 63% of those patients remaining asymptomatic.15 Asymptomatic colonization should not be treated, because antibiotics may further disrupt the gut microflora, potentially leading to symptomatic CDI.
Although increased stool output in a patient with history of CDI is concerning for RCDI, postinfectious irritable bowel syndrome (PI-IBS) should be kept in the differential diagnosis. PI-IBS occurs in approximately 25% of patients after successful CDI therapy.16 The distinction between RCDI and PI-IBS is not always apparent. However, patients with PI-IBS typically present with increased frequency in bowel habits with formed/solid stools (Bristol types 1 through 5). CDI testing should only be performed in patients having at least 3 Bristol type 6 or 7 stools per day or radiographic evidence of CDI.17
Three major medical societies have published guidelines for the treatment of RCDI: the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA) in 2010,11 the American College of Gastroenterology (ACG) in 2013,12 and the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) in 2014.13 Although these guidelines are very helpful, they are becoming outdated. In the meantime, new therapeutic measures have emerged, and other therapeutic options are in development that may change clinical practice in the near future.
Presented here are 2 case reports of RCDI in which the currently available and possible future therapies for RCDI are discussed.
NEXT: Case 1 and Discussion
Case 1
A 76-year-old man with a past medical history of diabetes, lung cancer (for which he was on a chemotherapy regimen), and RCDI (3 times in the past 4 months) presented to a hospital with a 2-week history of watery diarrhea (Bristol type 7). The diarrhea had occurred up to 10 times a day.
At presentation, his vital signs were stable, and he was afebrile. There was no abdominal tenderness or distention. Laboratory test results showed a peripheral white blood cell (WBC) count of 12,000/µL, a serum creatinine level of 0.9 mg/dL, and a serum albumin level of 3.5 g/dL. EIA test results are positive for C difficile toxin. The patient received a diagnosis of RCDI of mild-to-moderate severity, and he was started on enteral vancomycin, 125 mg 4 times daily. By hospital day 3, his diarrhea had resolved. Upon discharge, 14 days of vancomycin were prescribed.
Now the man has come to your clinic for a posthospitalization follow-up visit. He says he is doing well on vancomycin, but he is eager to stop taking the medication.
Discussion
This patient has multiple risk factors for RCDI: advanced age, chemotherapy, and a history of RCDI. The diagnosis of RCDI in this case is straightforward in the presence of Bristol type 7 diarrhea up to 10 times a day with positive toxin on EIA. Furthermore, the patient responded well to oral vancomycin; thus, a fourth episode of RCDI is confirmed.
After making a diagnosis, the severity of CDI needs to be assessed (Table 1). Severe CDI is characterized by a WBC count of 15,000/µL or greater, a serum albumin level of 3 g/dL or less, and/or a serum creatinine level of 1.5 times or more the premorbid level.11-13 In severe and complicated CDI cases, fever, lactic acidosis, overt leukocytosis/leukopenia, hypotension, shock, ileus, and/or megacolon may be present. Our patient’s case is classified as mild-to-moderate disease.11-13

The 3 widely recognized antimicrobial options in the treatment of CDI are metronidazole, vancomycin, and fidaxomicin. Ten-day supplies of each antibiotic therapy vary in cost: As of 2013, the cost of metronidazole was $22; the cost of vancomycin, 125 mg intravenous (IV), compounded for oral administration, ranged from $100 to $400; the cost of vancomycin, 125-mg pills, was $680; and the cost of fidaxomicin was $2,800.12 Metronidazole is the first-line agent for CDI and is available in oral and IV forms. Vancomycin has been used extensively and can be administered orally or via enema. To reduce cost, many pharmacies compound IV vancomycin solution to oral formulation. Guidelines recommend vancomycin doses varying from 125 to 500 mg, 4 times a day11-13; however, evidence suggests that 125 mg is equally efficacious compared with higher doses.18 Two recent meta-analyses showed that both metronidazole and vancomycin are equally efficacious in mild CDI, whereas vancomycin was superior in severe CDI.19,20
No convincing data suggest superiority of the combination of metronidazole and vancomycin compared with vancomycin monotherapy. However, it is still reasonable to use both high-dose enteral vancomycin (oral or rectal) and IV metronidazole in severe-complicated cases.
Fidaxomicin, a macrocyclic antibiotic with selective bactericidal activity against C difficile but negligible activity against gram-negative organisms, debuted in a 2011 landmark trial in which it was found to be noninferior to oral vancomycin.21 Furthermore, fidaxomicin appeared to be more effective than oral vancomycin in preventing relapse (28.1% vs 10.3%; P <.001), leading to better clinical cure rates.21 The 2014 ESCMID guidelines recommend the use of fidaxomicin in all CDI severities.13 Nevertheless, debate is ongoing about this medication, given the lack of indication in US guidelines, cost-effectiveness, and hospital formulary inclusion.
Guidelines for RCDI treatment have been evolving. The 2010 SHEA/IDSA guidelines11 recommend repeating the same antibiotic used for the initial episode for the first recurrence; for the second recurrence, pulsed or tapered vancomycin is recommended (Table 2). Three clinical trials have shown that vancomycin taper resulted in recurrence rates of 0% to 41.7%.4,22,23 The 2013 ACG guidelines added fecal microbiota transplant (FMT) plus vancomycin at the third recurrence.12 The 2014 ESCMID guidelines added fidaxomicin as an option in the first recurrence or subsequent recurrences.13 Less commonly, rifaximin, tigecycline, nitazoxanide, and linezolid are used.

Advances in CDI research have been rapid and multidirectional. FMT or “stool transplant” has emerged with the hypothesis that the disruption of the colonic microflora is the primary pathogenesis of CDI and that replacement of the microbiota with a more robust and diverse microbiota is a logical means to restore colonization resistance against C difficile. Numerous uncontrolled observational studies demonstrating cure rates of 90% or greater with FMT culminated in the landmark 2013 study in which significant efficacy and clinical cure rates with FMT led to early termination of the trial.24 To date, 6 randomized controlled trials of FMT have been conducted, with treatment success rates ranging from 44% to 94%.22,24-28
Although the efficacy of FMT is appealing, the esthetic issue (so-called yuck factor) in FMT remains. To overcome this challenge, frozen material and fecal bank systems have been implemented.26,27 The Food and Drug Administration (FDA) classifies human stool as a biological agent and has determined that its use in FMT therapy and other research should be regulated to ensure patient safety. To use FMT to treat RCDI, an investigational new drug permit is not required but is strongly encouraged, and one may be required in the future.29,30 A few live biotherapeutic microbiota preparations (eg, RBX2660, SER-109) are in development.31,32 These products aim to harness the effectiveness of FMT, but within a standardized regulated product for the treatment of RCDI.
In January 2017, the results of 2 landmark studies evaluating bezlotoxumab, an FDA-approved monoclonal antibody against C difficile toxin B, were published.33 These industry-funded, phase 3 trials compared the efficacy of bezlotoxumab with standard-of-care antibiotics alone for preventing RCDI. In the first trial, 17% of participants taking bezlotoxumab experienced RCDI during the 12-week study period compared with 28% of participants taking placebo. Findings were similar in the second trial. Common adverse reactions to bezlotoxumab were nausea, pyrexia, and headache. Cardiac disorders (eg, cardiac failure, myocardial infarction) were more common in bezlotoxumab-treated participants with a history of cardiac disorders; thus, among such patients, bezlotoxumab should be reserved for use when the benefit outweighs the risk. Alluring characteristics of bezlotoxumab include an overall safe profile, a long half-life (30 hours) enabling 1-time infusions, and modest efficacy, although bezlotoxumab was not found to be the magic bullet as had been anticipated. Further research is needed to determine which population of patients with RCDI would benefit most from the drug.
Several intriguing developments may change clinical practice. A C difficile vaccine study is under way.34 Not all strains of C difficile produce toxins. Colonization of nontoxigenic C difficile strains in the gastrointestinal tract has been shown to prevent CDI,35 and further clinical trials are ongoing to evaluate the role of nontoxigenic C difficile colonization. Additionally, other therapeutic candidates, including ridinilazole, ramoplanin, thuricin CD, and auranofin, are under investigation.36 A novel approach with administration of an antibiotic degrader (ribaxamase, a recombinant β-lactamase) and an antibiotic chelator (DAV132) is also under study. The intention of these agents is to neutralize unmetabolized antibiotic in the colon to protect gut microbiota.
Outcome of Case 1
The patient received a vancomycin taper: 125 mg orally 4 times a day for 14 days, then twice daily for 7 days, then daily for 7 days, then every 2 days for 8 days (4 doses), and finally every 3 days for 15 days (5 doses) as suggested in one review article.37 His condition improved, but CDI relapsed. He subsequently received FMT via enema, after which his RCDI finally resolved.
NEXT: Case 2 and Outcome
Case 2
The patient is a 36-year-old nurse with a past medical history of depression (for which she takes citalopram) and recurrent furuncles in her groin from methicillin-resistant Staphylococcus aureus (MRSA) infection. She also has a history of 2 episodes of RCDI in the past year. She had visited your office for treatment of another furuncle on her right buttock. Incision and drainage had been performed in your office. Wound cultures grew MRSA susceptible to trimethoprim-sulfamethoxazole (TMP-SMX), clindamycin, tetracycline, linezolid, and vancomycin.
She now visits your office for follow-up, and you note cellulitis surrounding the evacuated furuncle. You decide to start her on an oral antimicrobial agent. Although the woman does not have diarrhea now, she is concerned about having a flare of RCDI if an antibiotic is initiated. Which antimicrobial would you choose for MRSA cellulitis, and how best would you prevent RCDI in this patient’s case?
Discussion
Antibiotic use is one the most important risk factors for RCDI.38 However, some agents carry a higher risk than others (Table 3).39 Among anti-MRSA agents, clindamycin is associated with a higher rate of CDI, whereas TMP-SMX has a moderate risk for CDI. Tetracycline is not commonly associated with CDI.39,40 In the case of this patient with a history of RCDI, given her susceptibility test results and considering her history of and risk for RCDI, tetracycline would be the best choice.

Oral antimicrobials are generally equally efficacious to parenteral agents in mild to moderate skin and soft-tissue infections.41 However, parenteral agents are often recommended in severe cases. Linezolid may be an exception. It is available in oral and parenteral forms, and its bioavailability is almost 100%. Therefore, the dosing is the same in either formulation. A 2016 meta-analysis of all 9 available randomized trials showed that the clinical efficacy of linezolid is superior to IV vancomycin in skin and soft-tissue infections.42 Linezolid recently became a generic medication, resulting in a significant price reduction and making it more attractive as an efficacious antibiotic. Linezolid also is associated with a low risk of RCDI. However, the use of linezolid is often hindered by drug-drug interactions, including with selective serotonin-uptake inhibitors, tricyclic antidepressants, venlafaxine, tramadol, and antiemetics. Coadministration of linezolid with these medications may induce serotonin syndrome.43
Several RCDI prevention strategies are available in addition to the choice of antibiotic. Although data on their efficacy are limited, probiotics could be considered.44 Of note, probiotics should be used with caution in immunocompromised patients, given the possible risk of bacterial translocation, which occasionally causes disastrous outcomes.45
One study has shown that oral vancomycin, 125 mg twice daily, is effective for the prevention of RCDI while a patient is taking a concomitant antibiotic.46 In our practice, we usually extend the duration of prophylactic oral vancomycin up to 1 week beyond the stopping date of the primary infection (such as urinary tract infection or osteomyelitis).
Outcome of Case 2
The patient received oral doxycycline, 100 mg twice daily for 7 days, which led to resolution of the cellulitis. She also received prophylactic oral vancomycin, 125 mg twice daily for 14 days. There was no recrudescence of RCDI.
Eiyu Matsumoto, MB, is a clinical assistant professor in the Department of Internal Medicine, Division of Infectious Diseases, at the University of Iowa Carver College of Medicine in Iowa City, Iowa.
Jennifer R. Carlson, PA-C, is a physician assistant at the Iowa City Veterans Affairs Health Care System in Iowa City, Iowa.
Alice Xu, MD, is a third-year resident in the Department of Internal Medicine at University of Iowa Hospitals and Clinics in Iowa City, Iowa.
References:
- Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143(5):1179-1187.e1-3.
- Wiegand PN, Nathwani D, Wilcox MH, Stephens J, Shelbaya A, Haider S. Clinical and economic burden of Clostridium difficile infection in Europe: a systematic review of healthcare-facility-acquired infection. J Hosp Infect. 2012;81(1):1-14.
- McDonald LC, Coignard B, Dubberke E, Song X, Horan T, Kutty PK; Ad Hoc Clostridium difficile Surveillance Working Group. Recommendations for surveillance of Clostridium difficile–associated disease. Infect Control Hosp Epidemiol. 2007;28(2):140-145.
- Mcfarland LV, Elmer GW, Surawicz CM. Breaking the cycle: treatment strategies for 163 cases of recurrent Clostridium difficile disease. Am J Gastroenterol. 2002;97(7):1769-1775.
- Kamboj M, Khosa P, Kaltsas A, Babady NE, Son C, Sepkowitz KA. Relapse versus reinfection: surveillance of Clostridium difficile infection. Clin Infect Dis. 2011;53(10):1003-1006.
- Figueroa I, Johnson S, Sambol SP, Goldstein EJC, Citron DM, Gerding DN. Relapse versus reinfection: recurrent Clostridium difficile infection following treatment with fidaxomicin or vancomycin. Clin Infect Dis. 2012;55(suppl 2):S104-S109.
- Kyne L, Warny M, Qamar A, Kelly CP. Association between antibody response to toxin A and protection against recurrent Clostridium difficile diarrhoea. Lancet. 2001;357(9251):189-193.
- Abdelfatah M, Nayfe R, Nijim A, et al. Factors predicting recurrence of Clostridium difficile infection (CDI) in hospitalized patients: retrospective study of more than 2000 patients. J Investig Med. 2015;63(5):747-751.
- Surawicz CM, McFarland LV, Greenberg RN, et al. The search for a better treatment for recurrent Clostridium difficile disease: use of high-dose vancomycin combined with Saccharomyces boulardii. Clin Infect Dis. 2000;31(4):1012-1017.
- Wenisch C, Parschalk B, Hasenhündl M, Hirschl AM, Graninger W. Comparison of vancomycin, teicoplanin, metronidazole, and fusidic acid for the treatment of Clostridium difficile–associated diarrhea. Clin Infect Dis. 1996;22(5):813-818.
- Cohen SH, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31(5):431-455.
- Surawicz CM, Brandt LJ, Binion DG, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol. 2013;108(4):478-498.
- Debast SB, Bauer MP, Kuijper EJ. European Society of Clinical Microbiology and Infectious Diseases: update of the treatment guidance document for Clostridium difficile infection. Clin Microbiol Infect. 2014;20(suppl 2):1-26.
- Ozaki E, Kato H, Kita H, et al. Clostridium difficile colonization in healthy adults: transient colonization and correlation with enterococcal colonization. J Med Microbiol. 2004;53(pt 2):167-172.
- Barbut F, Petit J-C. Epidemiology of Clostridium difficile-associated infections. Clin Microbiol Infect. 2001;7(8):405-410.
- Wadhwa A, Al Nahhas MF, Dierkhising RA, et al. High risk of post-infectious irritable bowel syndrome in patients with Clostridium difficile infection. Aliment Pharmacol Ther. 2016;44(6):576-582.
- Gupta A, Khanna S. Repeat Clostridium difficile testing. JAMA. 2016;316(22):2422-2423.
- Fekety R, Silva J, Kauffman C, Buggy B, Deery HG. Treatment of antibiotic-associated Clostridium difficile colitis with oral vancomycin: comparison of two dosage regimens. Am J Med. 1989;86(1):15-19.
- Li R, Lu L, Lin Y, Wang M, Liu X. Efficacy and safety of metronidazole monotherapy versus vancomycin monotherapy or combination therapy in patients with Clostridium difficile infection: a systematic review and meta-analysis. PLoS ONE. 2015;10(10):e0137252. doi:10.1371/journal.pone.0137252
- Di X, Bai N, Zhang X, et al. A meta-analysis of metronidazole and vancomycin for the treatment of Clostridium difficile infection, stratified by disease severity. Braz J Infect Dis. 2015;19(4):339-349.
- Louie TJ, Miller MA, Mullane KM, et al; OPT-80-003 Clinical Study Group. Fidaxomicin versus vancomycin for Clostridium difficile infection. N Engl J Med. 2011;364(5):422-431.
- Hota SS, Sales V, Tomlinson G, et al. Oral vancomycin followed by fecal transplantation versus tapering oral vancomycin treatment for recurrent Clostridium difficile infection: an open-label, randomized controlled trial. Clin Infect Dis. 2017;64(3):265-271.
- Tedesco FJ, Gordon D, Fortson WC. Approach to patients with multiple relapses of antibiotic-associated pseudomembranous colitis. Am J Gastroenterol. 1985;80(11):867-878.
- van Nood E, Vrieze A, Nieuwdorp M, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013;368(5):407-415.
- Cammarota G, Masucci L, Ianiro G, et al. Randomised clinical trial: faecal microbiota transplantation by colonoscopy vs. vancomycin for the treatment of recurrent Clostridium difficile infection. Aliment Pharmacol Ther. 2015;41(9):835-843.
- Youngster I, Sauk J, Pindar C, et al. Fecal microbiota transplant for relapsing Clostridium difficile infection using a frozen inoculum from unrelated donors: a randomized, open-label, controlled pilot study. Clin Infect Dis. 2014;58(11):1515-1522.
- Lee CH, Steiner T, Petrof EO, et al. Frozen vs fresh fecal microbiota transplantation and clinical resolution of diarrhea in patients with recurrent Clostridium difficile infection: a randomized clinical trial. JAMA. 2016;315(2):142-149.
- Kelly CR, Khoruts A, Staley C, et al. Effect of fecal microbiota transplantation on recurrence in multiply recurrent Clostridium difficile infection: a randomized trial. Ann Intern Med. 2016;165(9):609-616.
- US Food and Drug Administration, Center for Biologics Evaluation and Research. Enforcement Policy Regarding Investigational New Drug Requirements for Use of Fecal Microbiota for Transplantation to Treat Clostridium difficile Infection Not Responsive to Standard Therapies: Draft Guidance for Industry. http://www.fda.gov/downloads/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformation/Guidances/Vaccines/UCM488223.pdf. Published March 2016. Accessed September 18, 2017.
- Infectious Diseases Society of America. Fecal microbiota transplantation: investigational new drug protocol. http://www.idsociety.org/FMT/. Accessed September 18, 2017.
- Orenstein R, Dubberke E, Hardi R, et al; PUNCH CD Investigators. Safety and durability of RBX2660 (microbiota suspension) for recurrent Clostridium difficile infection: results of the PUNCH CD study. Clin Infect Dis. 2016;62(5):596-602.
- Lagier J-C, Cadoret F, Raoult D. Critical microbiological view of SER-109. J Infect Dis. 2017;215(1):161-162.
- Wilcox MH, Gerding DN, Poxton IR, et al; MODIFY I and MODIFY II Investigators. Bezlotoxumab for prevention of recurrent Clostridium difficile infection. N Engl J Med. 2017;376(4):305-317.
- Sheldon E, Kitchin N, Peng Y, et al. A phase 1, placebo-controlled, randomized study of the safety, tolerability, and immunogenicity of a Clostridium difficile vaccine administered with or without aluminum hydroxide in healthy adults. Vaccine. 2016;34(18):2082-2091.
- Gerding DN, Meyer T, Lee C, et al. Administration of spores of nontoxigenic Clostridium difficile strain M3 for prevention of recurrent C difficile infection: a randomized clinical trial. JAMA. 2015;313(17):1719-1727.
- Trubiano JA, Cheng AC, Korman TM, et al. Australasian Society of Infectious Diseases updated guidelines for the management of Clostridium difficile infection in adults and children in Australia and New Zealand. Intern Med J. 2016;46(4):479-493.
- Kelly CP, LaMont JT. Clostridium difficile—more difficult than ever. N Engl J Med. 2008;359(18):1932-1940.
- Baxter R, Ray GT, Fireman BH. Case-control study of antibiotic use and subsequent Clostridium difficile-associated diarrhea in hospitalized patients. Infect Control Hosp Epidemiol. 2008;29(1):44-50.
- Brown KA, Khanafer N, Daneman N, Fisman DN. Meta-analysis of antibiotics and the risk of community-associated Clostridium difficile infection. Antimicrob Agents Chemother. 2013;57(5):2326-2332.
- Doernberg SB, Winston LG, Deck DH, Chambers HF. Does doxycycline protect against development of Clostridium difficile infection? Clin Infect Dis. 2012;55(5):615-620.
- Aboltins CA, Hutchinson AF, Sinnappu RN, et al. Oral versus parenteral antimicrobials for the treatment of cellulitis: a randomized non-inferiority trial. J Antimicrob Chemother. 2015;70(2):581-586.
- Yue J, Dong BR, Yang M, Chen X, Wu T, Liu GJ. Linezolid versus vancomycin for skin and soft tissue infections. Cochrane Database Syst Rev. 2016;(1):CD008056. doi:10.1002/14651858.CD008056.pub3
- Gupta V, Karnik ND, Deshpande R, Patil MA. Linezolid-induced serotonin syndrome. BMJ Case Rep. 2013;2013. doi:10.1136/bcr-2012-008199
- Lau CSM, Chamberlain RS. Probiotics are effective at preventing Clostridium difficile-associated diarrhea: a systematic review and meta-analysis. Int J Gen Med. 2016;9:27-37. doi:10.2147/IJGM.S98280
- Mehta A, Rangarajan S, Borate U. A cautionary tale for probiotic use in hematopoietic SCT patients—Lactobacillus acidophilus sepsis in a patient with mantle cell lymphoma undergoing hematopoietic SCT. Bone Marrow Transplant. 2013;48(3):461-462.
- Bajrovic V, Sims M. Vancomycin as prophylaxis of relapsing Clostridium difficile infection. Open Forum Infect Dis. 2016;3(suppl 1):2109. doi:10.1093/ofid/ofw172.1657


