Peer Reviewed
Bilateral Lymphadenopathy, Splenomegaly, and Hypercalcemia
A 46-year-old male presented with a history of intermittently increasing dyspnea on exertion over the past 3 years. On general appearance, the patient was comfortable at rest and in no acute distress.
Physical examination. The patient had a pulse of 74 beats per minute, blood pressure of 120/82 mm Hg, resting rate of 16 breaths per min, a temperature of 96.8°F, and oxygen saturation at 96% on room air.
Lung examination was unremarkable except for fine bilateral crackles. Cardiac examination revealed normal first and second heart sounds with no murmurs, friction, rub, or gallop. The abdomen was soft, with normal bowel sounds. The spleen could be palpated.
Neurological examination revealed that the cranial nerves were intact and there was no sensory or motor deficit.
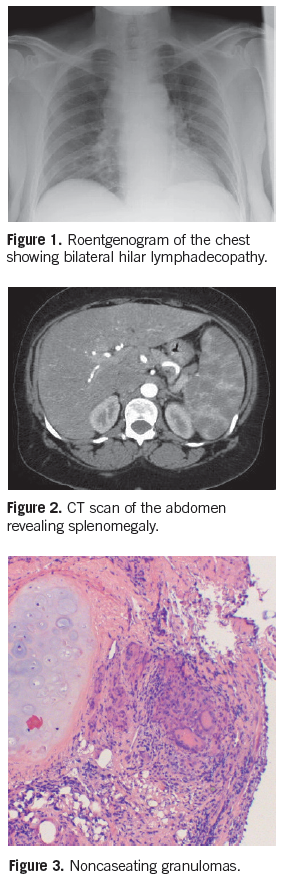
Roentgenogram of the chest revealed bilateral hilar lymphadenopathy (Figure 1). A CT scan of the abdomen also revealed splenomegaly (Figure 2). The patient denied any constitutional symptoms of fever, night sweats, malaise, or weight loss.
Laboratory tests. These were significant for an angiotensin-converting enzyme level of 80 U/mL, erythrocyte sedimentation rate of 52 mm/hour, and serum calcium levels were elevated to 12 mg/dL. The serum parathyroid hormone level was 15 pg/mL (normal 11-54 pg/mL).
Diagnosis. Our patient underwent a bronchoscopy and endobronchisl biopsy, which revealed evidence of noncaseating granulomas (Figure 3)—thereby suggesting sarcoidosis as cause of his symptomatology.
Discussion. Sarcoidosis is a systemic inflammatory disease of unknown etiology characterized by pathological hallmark of noncaseating granulomas. It commonly presents with bilateral hilar lymphadenopathy, dry cough, dyspnea, lung infiltration, and skin lesions. In addition to classic pulmonary symptoms, another sign of sarcoidosis is hypercalemia. Hypercalemia in the setting of sarcodiosis is often asymptomatic and presents on serum testing. Although a systemic disease, it predominately affects the intrathoracic lymph nodes and lungs, as well as the spleen and liver.
Sarcoidosis is a diagnosis of exclusion and as such, other infectious and noninfectious causes of granulomas need to be evaluated for and ruled out by obtaining a complete medical, occupational, environmental, and medication history as well as physical examination, followed by the appropriate diagnostic testing.1
The hypercalcemia occurs in about 10% of cases of sarcoidosis; hypercalciuria is 3 times more common. Calcium abnormalities may precede, follow, or appear at any time during the course of sarcoidosis. The primary defect involves excessive 1-alpha hydroxylation of 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D by the granulomatous tissue.2 This may lead to increased gut absorption of calcium, hypercalciuria, and hypercalcemia. If it is not treated, the patient may develop nephrocalcinosis, renal stones, or even renal failure.
Hypercalcaemia may be prevented by a low calcium diet, adequate hydration, and minimization of exposure to light. Milk, cheese, calcium-containing antacids, and vitamin D should be avoided. Corticosteroids are the mainstay of treatment for more severe hypercalcaemia, occurring despite these preventive measures. Prednisone, dosed at 20-40 mg/d, is the drug of choice to reduce the endogenous
production of 1,25(OH)2D3.3
The institution of corticosteroid therapy causes a relatively swift decrease in circulating 1,25(OH)2D3 and serum calcium level lower subsequently. If the patient develops unbearable side effects of corticosteroid therapy or fails to respond, hydrochloroquine4 may be an option. Hydroxychloroquine is also known to reduce serum 1,25(OH)2D3 and calcium concentrations. The antifungal drug ketoconazole, a known inhibitor of cytochrome P450 steroid oxidases, lowers circulating 1,25(OH)2D3 and serum calcium levels; however, its efficacy is not widely recognized.5
Outcome of the case. Our patient responded to prednisone, which was continued over the next 12 weeks andthen tapered slowly. His serum calcium remained normal.
References:
- Newman L, Rose C, Maier LA. Sarcoidosis. N Engl J Med. 1997;336:1224-1234.
- Sharma OP. Vitamin D, calcium and sarcoidosis. Chest. 1996;109(2);535-539.
- Adams J. Hypercalcemia and hypercalciuria. Semin Respir Med. 1992;13:402-410.
- Barre PE, Gascon-Barre M, Meakins J, et al. Hydroxychloroquine treatment of hypercalcemia in a patient with sarcoidosis undergoing hemodialysis. Am J Med. 1987; 82:1259-1632.
- Adams J, Sharma O, Diz M, et al. Ketoconazole decreases the serum 1,25-dihydroxy vitamin D and calcium concentration in sarcoidosis associated hypercalcemia.
- J Clin Endocrino Metab. 1990;70:1090-1095.


