Atypical Presentation of Acute Myocardial Infarction
A 58-year-old man presented with a sudden onset of dyspnea at rest. He had become nonverbal and had been intubated in the field due to hypoxia, with an oxygen saturation of 58% on room air.
History. No further history of present illness could be obtained. The patient had no known drug allergies. He also had prostate cancer, hypertension, hyperlipidemia, and bilateral peripheral vascular disease. His father has hypertension and hyperlipidemia. The patient has a 30 pack-year history of smoking, but he had quit 3 years prior. He has 3 or 4 alcoholic drinks a week.
Physical examination. Vital signs were as follows: blood pressure, 190/98 mm Hg; pulse, 136 beats/min; respiratory rate, 30 cycles/min; oxygen saturation, 83% on 15 L/min oxygen administered via bag valve mask. Cardiovascular and respiratory examination findings were normal, except for the presence of sinus tachycardia.
Diagnostic tests. His white blood cell count was 9,980/µL, his hemoglobin level was 11 g/dL, and his platelet count was 238 × 103/µL. The troponin I level was elevated at 0.06 ng/mL, and the B-type natriuretic peptide (BNP) level was 460 pg/mL. Electrocardiography (ECG) showed sinus tachycardia, left axis deviation, and left bundle branch block (Figure 1). No previous ECG was available for comparison.

Figure 1. Electrocardiogram showed sinus tachycardia, left axis deviation, and left bundle branch block.
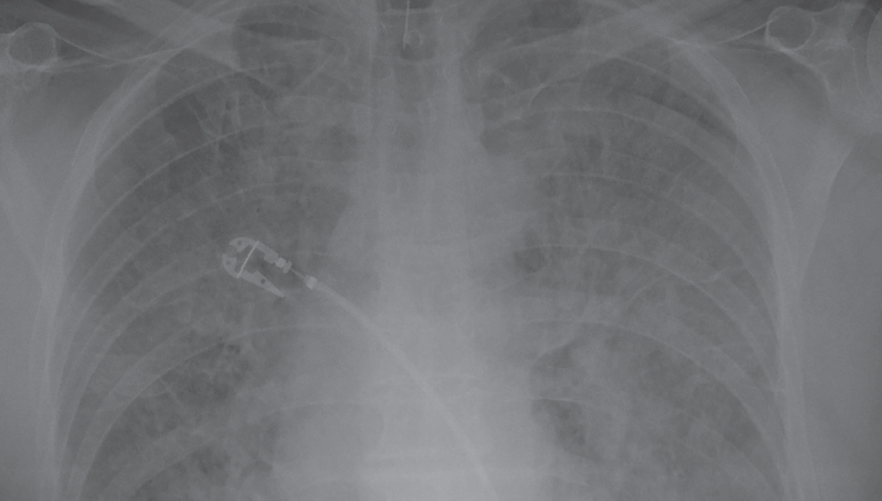
Figure 2. Anteroposterior chest radiograph showed diffuse opacity in the bilateral lung fields. The cardiac silhouette was within normal limits. The tip of an endotracheal tube is visible at the thoracic inlet.
Anteroposterior chest radiography (Figure 2) showed diffuse opacity in the bilateral lung fields. The cardiac silhouette was within normal limits.
Discussion. Coronary artery disease (CAD) is a major cause of morbidity and mortality in developed countries and was the cause of 1 in 6 deaths in the United States in 2006.1 Current guidelines state that patients with ST-elevation myocardial infarction (STEMI) should be treated with percutaneous coronary intervention (PCI) within 90 minutes of first medical contact; if PCI cannot be delivered during this time, and in the absence of contraindications, thrombolytic therapy should be administered within 30 minutes of presentation.2
However, these guidelines are not always applicable in clinical scenarios of STEMI, such as left bundle branch block (LBBB) as seen in this patient, paced rhythm, and in cases where a detailed history of angina symptoms cannot be obtained.3
Approximately 6.7% of patients with acute MI present with LBBB.4 LBBB can interfere with ECG interpretation and the diagnosis of an acute MI when the age of the LBBB is unknown. One group of researchers noted that chest pain was not present in half of patients with LBBB and an acute MI.5
The Sgarbossa criteria can be helpful in instances where a patient has LBBB but where access to patient history is limited or unable to be obtained, and where no prior ECG is available. The Sgarbossa criteria were proposed in 1996 as a scoring system graded on a scale of 0 to 5 to help determine the significance of LBBB in relation to an MI. The Sgarbossa score is based on 3 ECG criteria in the diagnosis of acute MI6:
- ST segment elevation of 1 mm or more that is in the same direction (concordant) as the QRS complex in any lead: score 5.
- ST segment depression of 1 mm or more in any lead from V1 to V3: score 3.
- ST segment elevation of 5 mm or more that is discordant with the QRS complex (ie, associated with a QS or rS complex): score 2.
The first criterion is reported to be more accurate for diagnosing an acute MI. However, this criterion has limitations, since the sensitivity of a Sgarbossa score of 3 or more is approximately 20%.6
Other possibly helpful ECG findings include the Cabrera sign, which is a prominent (0.05 sec) notching in the ascending limb of the S wave in leads V3 and V4; a similar finding is the Chapman sign, which is a prominent notching of the ascending limb of the R wave in lead V5 or V6.7 These signs have approximately 90% specificity. Notably, the sensitivity of these signs is low.7
Bedside echocardiography is another diagnostic options to help in making a quick decision in a case for reperfusion therapy in these instances. The presence of wall-motion abnormalities revealed by bedside echocardiography supports the presence of a STEMI. A management algorithm for patients with LBBB and suspected MI has been proposed.8
This is a case of MI with atypical presentation, since we could not elicit the typical symptoms such as left-sided chest pain because the patient was obtunded. However, the patient had dyspnea, risk factors for acute coronary syndrome (ACS), signs of fluid overload with bilateral opacity on chest radiographs, elevated troponin levels, and LBBB on ECG, all of which are highly suggestive of ACS.
Differential diagnosis. Among the other possible diagnoses was pulmonary edema, but this was less likely since ACS better explained the patient’s presentation. If a patient is not improving, and echocardiography and cardiac catheterization results are normal, obtaining a computed tomography angiography scan is a reasonable measure. Our patient did have elevated cardiac enzymes, but this can be seen in a patient with myocardial oxygen demand mismatch, such as in cases of demand ischemia or an acute MI.

Figure 3. A still image from cardiac catheterization showed the left anterior descending (LAD) artery with minor proximal disease/stenosis. The diagonal artery is a large vessel with a proximal 90% stenosis. There is moderate disease/stenosis in the diagonal artery proximate to the high-grade lesion up to the bifurcation with the LAD; this diagonal artery goes all the way to the apex.
Pneumonia is less likely, since this was a sudden presentation without cough, fever, or leukocytosis, although chest radiographs showed bilateral opacity. The opacity was most likely due to pulmonary edema leading to fluid overload. Aortic stenosis (AS) can present with dyspnea, usually of subacute to chronic onset. AS more commonly presents with angina and syncope. On echocardiography, stenosis of the aortic valve is seen.
Patients with flash pulmonary edema usually present with dyspnea, wheezing, decreased breath sounds, rales, rhonchi, and jugular venous distention. Our patient did have some of these features, along with an elevated BNP level and chest radiograph features consistent with congestive heart failure. However, pulmonary edema is a secondary diagnosis, and treating it alone will not address the root cause of the problem.

Figure 4. A still image from cardiac catheterization showing stent placement in the diagonal artery in the area of stenosis.

Figure 5. A still image echocardiographic image (2-dimensional and M-mode), a technically very difficult study with limited views, that shows normal left ventricular wall thickness. Right ventricular size also is normal.
Outcome of the case. The patient was started on furosemide for diuresis and standard CAD therapy. An echocardiogram showed wall motion abnormality (Figure 3). He was found to have multivessel CAD; he received a drug-eluting stent in the diagonal branch of the left coronary artery (Figures 4 and 5) during cardiac catheterization and was transferred to the intensive care unit for further management. The patient later was extubated successfully and discharged home with advice to follow-up with his primary care physician within a week. Discharge was 3 days after initial presentation.
References:
- Lloyd-Jones D, Adams RJ, Brown TM, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Executive summary: heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation. 2010;121(7):948-954.
- Kushner FG, Hand M, Smith SC Jr, et al. 2009 focused updates: ACC/AHA Guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2009;120(22):2271-1306.
- Mehta SR, Granger CB, Boden WE, et al; TIMACS Investigators. Early versus delayed invasive intervention in acute coronary syndromes. N Engl J Med. 2009;360(21):2165-2175.
- Go AS, Barron HV, Rundle AC, Ornato JP, Avins AL. Bundle-branch block and in-hospital mortality in acute myocardial infarction. Ann Intern Med. 1998;129(9):690-697.
- Shlipak MG, Go AS, Frederick PD, Malmgren J, Barron HV, Canto JG; National Registry of Myocardial Infarction 2 Investigators. Treatment and outcomes of left bundle-branch block patients with myocardial infarction who present without chest pain. J Am Coll Cardiol. 2000;36(3):706-712.
- Tabas JA, Rodriguez RM, Seligman HK, Goldschlager NF. Electrocardiographic criteria for detecting acute myocardial infarction in patients with left bundle branch block: a meta-analysis. Ann Emerg Med. 2008;52(4):329–336.e1.
- Wackers FJ. The diagnosis of myocardial infarction in the presence of left bundle branch block. Cardiol Clin. 1987;5(3):393-401.
- Neeland IJ, Kontos MC, de Lemos JA. Evolving considerations in the management of patients with left bundle branch block and suspected myocardial infarction. J Am Coll Cardiol. 2012;60(2):96-105.


