Peer Reviewed
Myxedema Coma
AUTHORS:
Adedeji Olusanya, DO1 • Ahmed Salim, DO1 • Karla Objio, MS-III1 • Syed A. A. Rizvi, PhD, MS, MBA2 • Wilson Pfeiffer, DO3 • Alixandria Pfeiffer, DO4 • Jose Paz, DO5
AFFILIATIONS:
1Nova Southeastern University, Fort Lauderdale, Florida
2Hampton University School of Pharmacy, Hampton, Virginia
3Brooke Army Medical Center, San Antonio, Texas
4University of Texas Health Science Center, San Antonio, Texas
5Palmetto General Hospital, Miami, Florida
CITATION:
Olusanya A, Salim A, Objio K, et al. Myxedema coma. Consultant. 2022;62(3):e6-e8. doi:10.25270/con.2021.04.00006
Received July 14, 2020. Accepted January 18, 2021. Published online April 13, 2021.
DISCLOSURES:
The authors report no relevant financial relationships.
CORRESPONDENCE:
Syed A. A. Rizvi, PhD, MS, MBA, Department of Pharmaceutical Sciences, Hampton University School of Pharmacy, 100 E Queen Street, Hampton, VA 23669 (syed.rizvi@hamptonu.edu)
A 77-year-old woman presented to the emergency department with shortness of breath. She had a medical history significant for chronic obstructive pulmonary disease, coronary artery disease, myocardial infarction status after coronary artery bypass grafting, atrial fibrillation, a permanent pacemaker, type 2 diabetes, obstructive sleep apnea, hypertension, and hypothyroidism.
She stated that her symptoms were exacerbated by lying down and improved upon sitting up. She also said that she has experienced chronic shortness of breath, but it had recently worsened. In addition, she reported mild, intermittent midsternal chest pain that radiated to her left arm and was associated with nausea.
Physical examination. The patient was morbidly obese but appeared to be in no acute distress. The examination findings demonstrated an irregular heart rhythm, a large neck circumference, a grade of 2+ for pitting edema bilaterally on the lower extremities, decreased active range of motion in the bilateral lower extremities, and stasis dermatitis bilaterally in the lower extremities with ulceration of left medial leg. The patient was afebrile without leukocytosis and was hemodynamically stable.
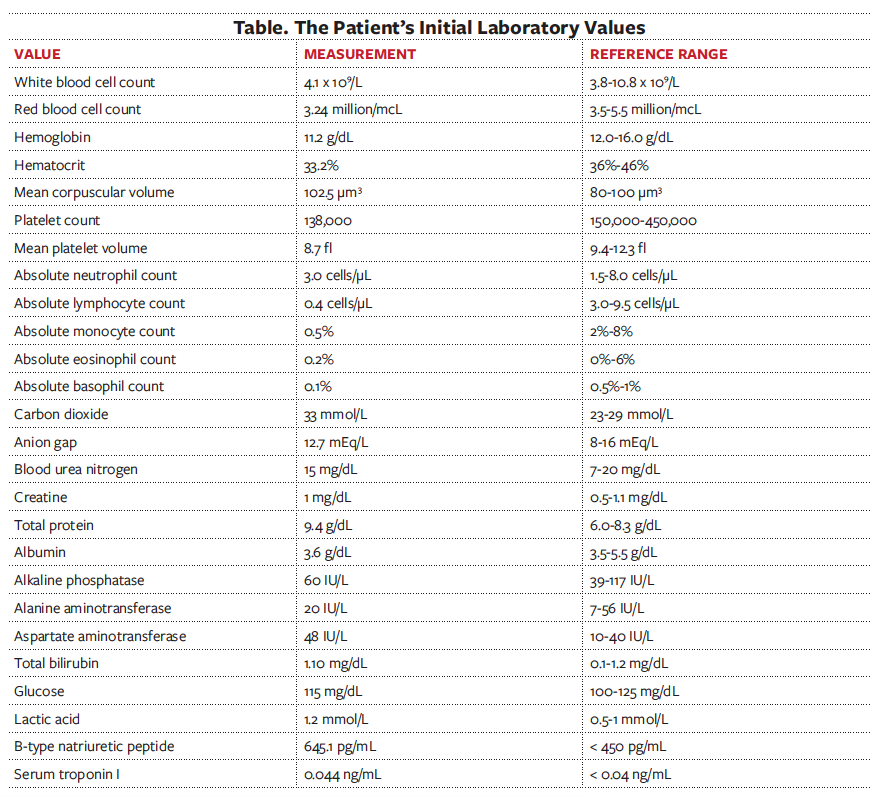
Laboratory testing. The results of the patient’s initial workup are listed in the Table. The patient was then transferred to step-down therapy and was then found obtunded on a bilevel positive airway pressure (BiPAP) machine. She was unresponsive to sternal rub. A new set of laboratory tests were ordered, results of which revealed an increase in pro- B-type natriuretic peptide of 3671 pg/mL (normal, < 450 pg/mL), thyroid-stimulating hormone (TSH) level greater than 100 (reference range, 0.4-4.0 mU/L), and T4 levels less than 0.40 μg/dL (reference range, 5-13.5 μg/dL). Results of a urine analysis and culture were negative, as were results of influenza, procalcitonin, and peptide nucleic acid studies.
Diagnostic testing. A bronchoscopy was performed that revealed a moderate amount of frothy secretions, without any evidence of an endobronchial mass, lesions, or a hemorrhage. Interrogation of the patient’s pacemaker demonstrated a malfunctioning atrial lead, with less than 1 month of generator life remaining. In addition, an echocardiography was performed that revealed the patient’s ejection fraction was 35% to 40% (reference range, 50%-70%). Diastolic examination suggested an elevated left atrial pressure; the left atrium was found to be mildly dilated, and there was mild mitral regurgitation, moderate tricuspid regurgitation, and severe pulmonary hypertension.
Discussion. Myxedema coma is defined as severe hypothyroidism, which can lead to several complications, including but not limited to hypothermia, altered mental status, hypoventilation, and organ failure. This rare, life-threatening problem is more common in women older than age 60 years and is estimated to affect 0.22 per million people per year.1-3 The term “myxedema” was devised by William Miller Ord4 to describe the common physical findings of generalized swelling, macroglossia, ptosis, periorbital edema, coarse, sparse hair, and nonpitting edema of lower extremities among women.5,6 Patients with myxedema coma typically have severe primary hypothyroidism with complications of low serum levels of thyroxine (T4) and triiodothyronine (T3) and high levels of TSH.7 Diagnosis can be confirmed with a TSH test, along with a T4 test.8
This crisis is considered a medical emergency, and treatment should be in an intensive care unit. In addition, treatment should consist of aggressive management of precipitating factors and thyroid hormone replacement. Prognosis is problematic to determine, as there are few reported cases in the literature.9 The severity of this condition, however, is clear. Some studies suggest that the mortality rate is as high as 60%, and therefore an important component in treatment is early recognition.10 There is often a high mortality rate associated with myxedema coma despite appropriate treatment and testing. This case demonstrates the significance of timely assessment and thorough evaluation of symptoms to optimize patient care.
Patient outcome. A treatment plan was formulated to target the set of symptoms. Respiratory failure, chronic obstructive pulmonary disease exacerbation, and obstructive sleep apnea were treated post-extubation with ipratropium bromide/albuterol, a long-acting β-agonist, inhaled corticosteroids, and continuous positive airway pressure at night. A congestive heart failure exacerbation was treated with diuresis (intravenous furosemide). Intravenous levothyroxine sodium was administered to treat the patient’s severe hypothyroidism. The patient was referred for an electrophysiology consultation and prescribed heparin drops for atrial fibrillation, complete atrioventricular block, and malfunctioning atrial lead on the pacemaker. In addition, she was advised to seek physical and occupational therapy and make dietary modifications.
References
1. Mathew V, Misgar RA, Ghosh S, et al. Myxedema coma: a new look into an old crisis. J Thyroid Res. 2011;2011:493462. https://doi.org/10.4061/2011/493462
2. Takamura A, Sangen R, Furumura Y, et al. Diagnosis of myxedema coma complicated by renal failure: a case report. Clin Case Rep. 2017;5(4):399-402. https://doi.org/10.1002/ccr3.850
3. Zhu Y, Qiu W, Deng M, Zhu X. Myxedema coma: a case report of pediatric emergency care. Medicine (Baltimore). 2017;96(21):e6952. https://doi.org/10.1097/MD.0000000000006952
4. Pearce JM. Myxoedema and Sir William Withey Gull (1816-1890). J Neurol Neurosurg Psychiatry. 2006; 77(5):639. https://dx.doi.org/10.1136%2Fjnnp.2005.082198
5. Wall CR. Myxedema coma: diagnosis and treatment. Am Fam Physician. 2000;62(11):2485-2490. https://www.aafp.org/afp/2000/1201/p2485.html
6. Gish DS, Loynd RT, Melnick S, et al Myxoedema coma: a forgotten presentation of extreme hypothyroidism. Case Rep. 2016;2016:bcr2016216225. https://doi.org/10.1136/bcr-2016-216225
7. Carter Y, Sippel RS, Chen H. Hypothyroidism after a cancer diagnosis: etiology, diagnosis, complications, and management. Oncologist. 2014;19(1):34-43. https://doi.org/10.1634/theoncologist.2013-0237
8. Popoveniuc G, Chandra T, Sud A, et al. A diagnostic scoring system for myxedema coma. Endocr Pract. 2014;20(8):808-817. https://doi.org/10.4158/EP13460.OR
9. Sethi P, Kamal M, Verma S, et al. Undiagnosed myxedema coma: rare but life-threatening. Saudi J Anaesth. 2018;12(1):173-174. https://doi.org/10.4103/1658-354X.222365
10. Dhakal P, Pant M, Acharya PS, et al. Myxedema coma with reversible cardiopulmonary failure: a rare entity in 21st century. Maedica (Buchar). 2015;10(3):268-271. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5327827/


